Das folgende Interview stellt einen Auszug aus meinem bald erscheinenden Buch „KREBS – verstehen, vermeiden und ganzheitlich behandeln“ dar, welches ingesamt zwölf derartige Interviews mit renommierten Therapeuten, Ärzten und Wissenschaftlern enthält.
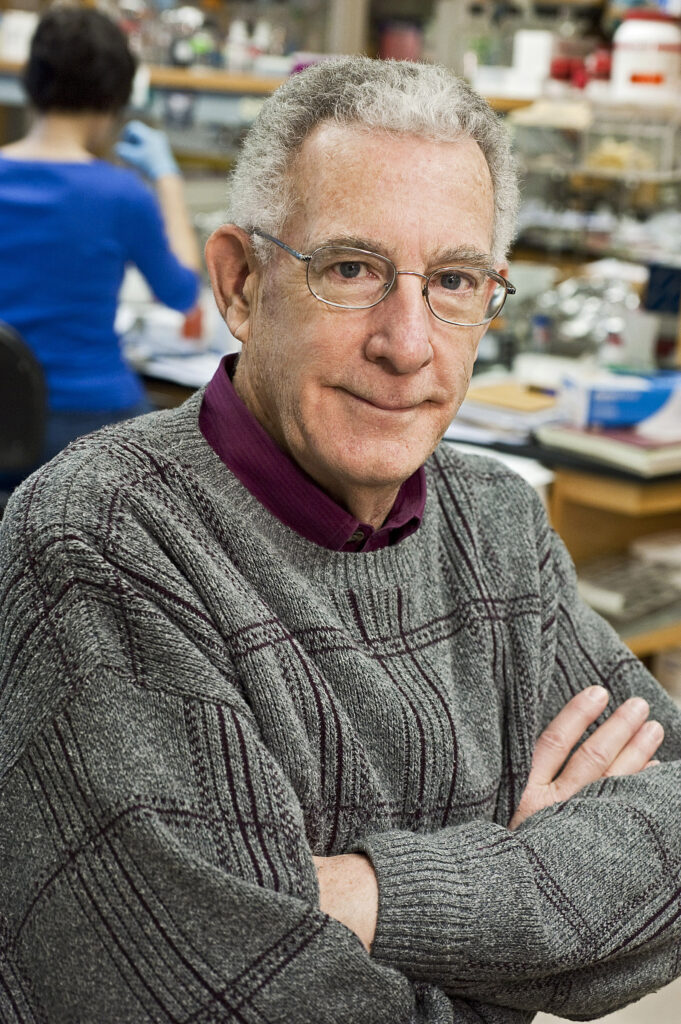
Thomas N. Seyfried ist Professor für Biologie am Boston College im US Bundesstaat Massachusetts; er promovierte 1976 in Genetik und Biochemie an der Illinois Universität in der Stadt Urbana.
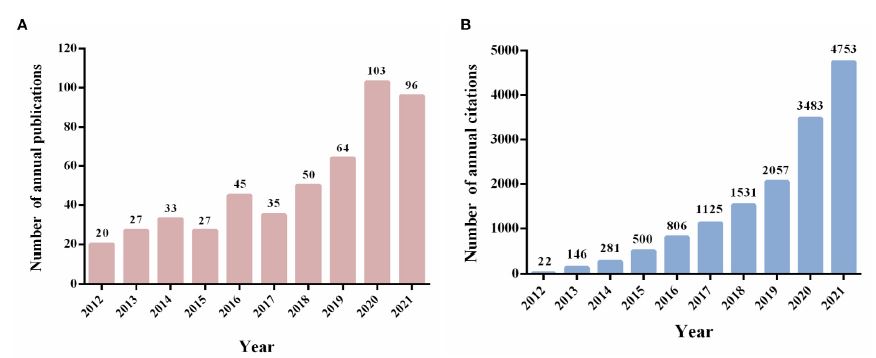
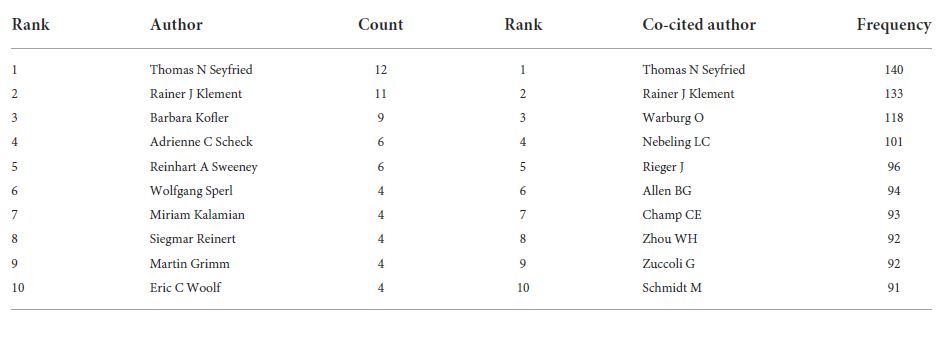
Sein Studium absolvierte er an der New England Universität, wo er vor kurzem den angesehenen Alumni Achievement Award verliehen bekam. Er besitzt auch einen Masterabschluss in Genetik von der Illinois Universität in der Stadt Normal im Zentrum von Illionois. Thomas Seyfried diente während dem Vietnamkrieg in der ersten Kavallerie-Division der US Army, wo er mehrfach mit Medaillen und Empfehlungsschreiben ausgezeichnet wurde. Er war wissenschaftlicher Mitarbeiter in der Abteilung für Neurologie an der medizinischen Fakultät der Yale Universität, wo er sich auch zum Assistenzprofessor habilitierte. Andere Auszeichnungen und Ehrungen wurden ihm von verschiedensten Organisationen verliehen, darunter die American Oil Chemists Society, das National Institute of Health, die amerikanische Gesellschaft für Neurochemie und der speziellen Interessengruppe für ketogene Diäten der amerikanischen Epilepsiegesellschaft. Dr. Seyfried war früher Vorsitzender des wissenschaftlichen Beirats der nationalen Tay-Sachs and Allied Diseases Association. Für sein Lebenswerk wurde er von der Akademie für komplementäre und integrative Medizin und der internationalen Dose Response Society ausgezeichnet, und für seine Krebsforschungen erhielt er den Wissenschaftspreis des American College of Nutrition. Derzeit gehört er mehreren Redaktionsleitungen an, unter anderem für die Fachzeitschriften Nutrition & Metabolism, Neurochemical Research, dem Journal of Lipid Research, und ASN Neuro, wo er der Chefredakteur ist. Dr. Seyfried hat mehr als 200 wissenschaftliche Publikationen veröffentlicht und ist Autor des Buches Cancer as a Metabolic Disease: On the Origin, Management, and Prevention of Cancer (Wiley Press). Sein Buch wurde vor Kurzem ins Chinesische übersetzt und eine türkische Übersetzung ist in Arbeit. Er hat seine Forschung in vielen Podcasts und Radiointerviews beschrieben, und seine Arbeit bildet die Grundlage für den Dokumentarfilm The Cancer Revolution. Eine komplette Auflistung der wissenschaftlichen Publikationen von Dr. Seyfried kann in der medizinischen Literaturdatenbank PubMed aufgerufen werden (https://pubmed.ncbi.nlm.nih.gov).
Lieber Tom, vor 100 Jahren veröffentlichte Otto Warburg seine bahnbrechenden Forschungsergebnisse zum Tumorstoffwechsel, nach denen generell alle aggressiven Tumore durch eine hohe Aufnahme von Glukose bei gleichzeitig vermehrter Freisetzung von Laktat gekennzeichnet sind. Wann und warum hast Du ein Interesse an Warburg’s Arbeiten entwickelt?
Das war, als ich begann, Forschungen zur therapeutischen Wirkung von Kalorienrestriktion und kalorienbeschränkter ketogener Diäten bei Mäusen mit Hirntumoren durchzuführen. Wir fanden heraus, dass die therapeutischen Effekte dieser Behandlungen direkt mit einer Senkung des Blutzuckerspiegels und einer Erhöhung der Ketonkörper zusammenhingen. Warburg lieferte die Hinweise, dass alle Krebszellen die aerobe Fermentation von Glukose erhöhen, da ihre Fähigkeit der oxidativen Phosphorylierung (=Zellatmung) vermindert ist. Wir fanden auch heraus, dass alle häufigen Krebsarten durch Abnormitäten in der Anzahl, Struktur und Funktion ihrer Mitochondrien gekennzeichnet sind. Somit haben wir Warburg‘s Schlussfolgerungen bestätigt. Warburg hatte absolut Recht, als er Krebs als eine Störung der mitochondrialen Funktion definierte. Wir berichtigen aktuell ein paar Fehldeutungen, die im Zusammenhang mit Warburg’s Ergebnissen verbreitet wurden und sammeln neue Informationen, die Warburg damals nicht zur Verfügung standen, die aber die Neuformulierung der Theorie von Krebs als mitochondriale Stoffwechselerkrankung ermöglichen.
Kannst Du ein paar dieser Fehldeutungen von Warburg’s Ergebnissen benennen und kurz erklären?
Hier sind die Fehlinterpretationen, die Warburg in Bezug auf die ATP-Erzeugung in Krebszellen gemacht hat, und die Richtigstellungen dazu.
1. Warburg verwendete die Milchsäureproduktion als Maß für die ATP-Menge, die in Krebszellen durch Glykolyse erzeugt wird. Er nahm an, dass 1 mol Laktat äquivalent zu der Produktion von 1 mol ATP wäre. Er wusste nicht, dass viele Krebszellen große Mengen der Pyruvatkinase M2 (PKM2)-Isoform exprimieren, welche nicht wie die PKM1-Isoform im letzten Schritt der Glykolyse durch die Umwandlung von Phosphoenolpyruvat in Pyruvat ATP erzeugt (sie verursacht einen Rückstau in der Glykolyse, so dass deren Zwischenprodukte zur Nukleinsäure-, Phospholipid- und Aminosäure-Synthese abgezweigt werden). Krebszellen produzieren deshalb eine erhebliche Mange Laktat, unabhängig von der ATP-Synthese. Es ist insbesondere schwierig, das in der Glykolyse produzierte ATP in Krebszellen zu messen, die eine Mischung aus den PKM2 & PKM1 Isoformen haben. Also lag Warburg falsch, als er die Laktatproduktion als Maß für die ATP Synthese in der Glykolyse benutzte.
2. Warburg nahm auch an, dass der Sauerstoffverbrauch von Tumorzellen komplett mit der ATP Synthese durch oxidative Phosphorylierung korrelieren würde. Er rechnete aus, dass pro 1 mol verbrauchtem Sauerstoff 7 mol ATP durch oxidative Phosphorylierung erzeugt würden. Obwohl in normalen Zellen und Geweben der Sauerstoffverbrauch gut mit der ATP Erzeugung korreliert, zeigen neuere Daten aus mehreren Studien, dass in Krebszellen der Sauerstoffverbrauch nur teilweise mit einer ATP Erzeugung durch oxidative Phosphorylierung korreliert. Der größte Teil des verbrauchten Sauerstoffs in Krebszellen entfällt auf die Produktion von ROS und andere sauerstoffverbrauchenden Reaktionen, die unabhängig von der oxidativen Phosphorylierung sind. Darum lag Warburg falsch, als er den Sauerstoffverbrauch von Krebszellen als Maß für das durch oxidative Phosphorylierung erzeugte ATP benutzte.
3. Schließlich wusste Warburg nichts von der Möglichkeit, ATP aus Glutamin zu erzeugen, was innerhalb der Glutaminolyse auf Stufe des Succinyl-Coenzym A durch mitochondriale Substratebenenphosphorylierung passiert (Anmerkung: Succinyl-Coenzym A entsteht im katabolen Stoffwechselweg der Glutaminolyse aus α-Ketoglutarat, siehe Abbildung 14). Die Erzeugung von ATP durch Glutaminolyse kann eine unzureichende ATP-Produktion sowohl durch Zellatmung als auch durch Glykolyse kompensieren. Sowohl Warburg als auch sein Hauptkritiker Sidney Weinhouse wussten nicht über Glutaminfermentation als wichtige Quelle von ATP in Krebszellen Bescheid. Daraus folgt, dass die Argumente zwischen Warburg und Weinhouse, die sich auf Berechnungen der ATP Synthese durch den Meyerhof-Quotient bezogen, belanglos sind.
Warburg lag vollkommen richtig, indem er Krebs als Störung des mitochondrialen Energiestoffwechsels definierte, die eine kompensatorische Fermentation zur ATP-Gewinnung notwendig macht. Er fehldeutete nur die Laktatproduktion und den Sauerstoffverbrauch als zuverlässige Maße für die ATP-Produktion durch Glykolyse bzw. oxidative Phosphorylierung. Da zur damaligen Zeit kaum Daten zur Möglichkeit der ATP-Synthese durch mitochondriale Substratebenenphosphorylierung vorlagen, wusste Warburg nichts von dieser zweiten Möglichkeit der Fermentation, die ohne Sauerstoff, oxidative Phosphorylierung und Glykolyse ATP erzeugen kann. Warburg lag dahingehend richtig, dass er behauptete, aerobe Fermentation (=Fermentation trotz normaler Sauerstoffversorgung) würde eine unzureichende oxidative Phosphorylierung kompensieren.
In modernen Gesellschaften ist Krebs zu einer Art Pandemie ausgeartet. Welches sind die wichtigsten Risikofaktoren für die Krebsentstehung? Ist Fleisch ein Risikofaktor?
Ernährung und Lebensstil sind die wichtigsten Risikofaktoren für die Krebsentstehung. Der Verzehr hochverarbeiteter kohlenhydratreicher Lebensmittel bei gleichzeitigem Fehlen eines angemessenen täglichen körperlichen Trainings sind die hauptsächlichen Risikofaktoren für die meisten chronischen Krankheiten inklusive Krebs, Herz-Kreislauf-Erkrankungen, Typ 2-Diabetes, Übergewicht, Demenz und anderen. Übergewicht hat das Rauchen als wichtigen Risikofaktor für Krebs nun abgelöst.
Der Verzehr von natürlichem Fleisch ist kein Risikofaktor für Krebs. Unsere steinzeitlichen Vorfahren ernährten sich hauptsächlich von Fleisch, wie Du ja auch in diesem Buch beschrieben hast. Krebs ist unter indigenen Stämmen extrem selten, solange sie ihrem ursprünglichen Lebensstil folgen. Ohne Fleischkonsum in unserer evolutionären Vergangenheit würden wir heute nicht als menschliche Spezies existieren. Fleisch enthält kaum Kohlenhydrate. Von unserer Biologie her sind wir hervorragend an Fleischkonsum angepasst.
Kannst Du kurz beschreiben, was die wesentlichen Veränderungen sind, die während dem Übergang einer normalen Zelle in eine Krebszelle passieren?
Jede chronische Verletzung unserer Gewebe, die eine Schädigung der oxidativen Phosphorylierung in den Mitochondrien zur Folge hat, kann eine normale in eine Krebszelle verwandeln. Zu diesen Verletzungen zählen chronische Entzündungen, zeitweilige Hypoxie, Aussetzung gegenüber Karzinogenen oder Strahlung, Infektion mit onkogenen Viren, seltene vererbte Mutationen und der Alterungsprozess. Die Funktion der Mitochondrien kontrolliert die Zelldifferenzierung und den Zellzyklus. Die schrittweise Ersetzung der ATP-Erzeugung mittels oxidativer Phosphorylierung durch ATP-Erzeugung mittels Fermentation führt zu einer Entdifferenzierung und zur Fehlregulation des Zellwachstums. Eine Fehlregulation des Zellwachstums entspricht der offiziellen Definition von Krebs.
Gibt es Deiner Erfahrung nach einen relativen Unterschied zwischen Glukose und Glutamin hinsichtlich der Wichigkeit für Tumorzellen und falls ja, von welchen Faktoren hängt dieser ab?
Beide Substrate sind notwendig und hinreichend für die Lebensfähigkeit und das Wachstum der meisten, wenn nicht sogar aller Tumorzellen. Kohlenstoff aus Glukose befeuert die Glykolyse und den Pentosephosphatweg zur Erzeugung von Biomasse, während Glutamin die Glutaminolyse antreibt und Stickstoff für die Sythese von DNA, RNA und Proteinen liefert. Beide Substrate unterstützen auch die Erzeugung von ATP durch Substratebenenphosphorylierung (=Fermentation) im Zytoplasma bzw. den Mitochondrien. Wir haben bis heute weder eine Tumorzelle finden können, die im Stande war, längerfristig ohne Glukose oder Glutamin zu überleben, noch konnten wir eine Zuckerverbindung, Fettsäure oder Aminosäure finden, die einer Tumorzelle das Überleben ohne Glukose und Glutamin ermöglicht hat.
Kannst Du kurz das von Dir empfohlene Behandlungsprotokoll für Krebspatienten vorstellen?
Wir verwenden die therapeutische Press-Pulse-Strategie, um die Verfügbarkeit von Glukose und Glutamin für Tumorzellen einzuschränken. Tumorzellen können in Abwesenheit von Glukose und Glutamin weder Fettsäuren noch Ketonkörper für ihr Überleben nutzen. Daraus folgt im Rahmen der mitochondrialen Stoffwechseltheorie, dass die einfachste Strategie um Krebs in den Griff zu bekommen in einer Einschränkung der Verfügbarkeit von Glukose und Glutamin mit gleichzeitigem Wechsel in einen ketogenen Zustand besteht.
Was sind Deiner Meinung nach die wichtigsten Gründe dafür, dass es Therapien, die beim Stoffwechsel ansetzen, noch nicht in die klinische Anwendung geschafft haben und von vielen Onkologen sogar abgelehnt werden?
Die meisten Onkologen unterstützen solche Stoffwechseltherapien nicht, weil sie große Wissenslücken über die Biologie von Krebs besitzen und unbedingt den Status Quo aufrechterhalten wollen.
Ich habe auch gehört, wie Du darüber gesprochen hast, dass der menschliche Körper ein enormes Potential zur Selbstheilung besitzt und dass Gebete diesen Prozess noch verbessern können. Kannst Du das genauer erklären?
Der menschliche Körper kann sich selbst heilen, wenn er die Möglichkeit dazu bekommt. Die Einschränkung der Nahrung hat bei den meisten Säugetieren heilsame Effekte. Menschen scheinen die einzigen Säugetiere zu sein, die einfach weiter essen, wenn sie krank oder verletzt sind. Es ist lange bekannt, dass Fasten, während dem nur Wasser getrunken wird, sehr heilsame Effekte hat. Beten liefert die Kraft, ein solches Fasten diszipliniert durchzuhalten.
Ich erinnere mich voll Freude zurück an unsere gemeinsame Kneipentour 2017 in Tampa, Florida, wo wir Bier, Wein oder andere Getränke hatten (die genauen Details weiß ich nicht mehr…). Scheinbar teilen wir beide die Ansicht, dass für jemand, der gesund ist, keine Notwendigkeit besteht, übermäßig streng bei der Ernährung oder anderen Lebensstilfaktoren aufzupassen, und dass sozialer Austausch sehr wichtig ist. Was sind Deine 5-10 besten Ratschläge für ein langes gesundes Leben?
Das hier sind nur Anregungen:
1. Arbeite solange Du kannst und solange Dir die Arbeit Spaß macht.
2. Pflege Deine sozialen Kontake.
3. Achte auf Dein Körpergewicht, so dass der BMI innerhalb des Normalbereichs bleibt.
4. Trainiere täglich, um eine gute Herz-Kreislauffunktion zu erhalten.
5. Am wichtigsten: Versuche den Konsum von hochverarbeiteten kohlenhydratreichen Nahrungsmitteln zu vermeiden!